Portfolio
Avoiding recurrence by bio-modulation of hydroxyapatite
Deep bone infection is the most serious complication in orthopaedic surgery. In these infections, achieving an adequate local concentration of antibiotics is a challenge. Using the current treatment methods like long-term systemic antibiotics following local debridement, effective antibiotic levels may not reach the desired target and also lead to serious toxicities and the selection of antibiotic-resistant bacteria. Excellent long-term outcome has been reported in chronic osteomyelitis by radical debridement and filling the dead space with a gentamycin containing calcium sulphate/ hydroxyapatite (CaS/HA) bone substitute. High local concentrations can be reached by the elution of the antibiotic concomitant with the resorption of calcium sulphate during the first postoperative weeks. However, in extensive infections, sessile bacteria may remain in bone cells and adjacent cortical bone or soft tissue protected by biofilm and lead to recurrences.
In order to shorten the antibiotic treatment and to achieve high concentrations at MIC levels, surgeons in the last few decades have used local delivery of antibiotics added to PMMA bone cements. However, antibiotic containing PMMA does not give sustained release and lacks bone regeneration properties. No biomaterial however currently contains and delivers Rifampicin, an apatite binding antibiotic considered as cornerstone second defence antibiotic in the treatment of severe longstanding deep bone and joint prosthetic infections.
We are exploring a novel solution by delivering specific apatite binding antibiotics using bone regenerating carriers containing particulate nano and micro apatite particles. This could achieve clinically relevant local concentrations evading systemic side effects and prevent relapses of infection and at the same time build bone in a surgically eradicated bone infection defect.
1.3 million
trochanteric fracture in a year.
2%
of the cases are reported (3-7% require revision surgery due to failure in trochanteric fractures) to have a postoperative infection.
50%
1-year mortality rate of operated hip fractures with infection compared to 24 % with no infection.
‘Antibiotic recharging of locally implanted synthetic HA carriers at predetermined time intervals opens-up a new treatment modality in deep bone and joint infections’.
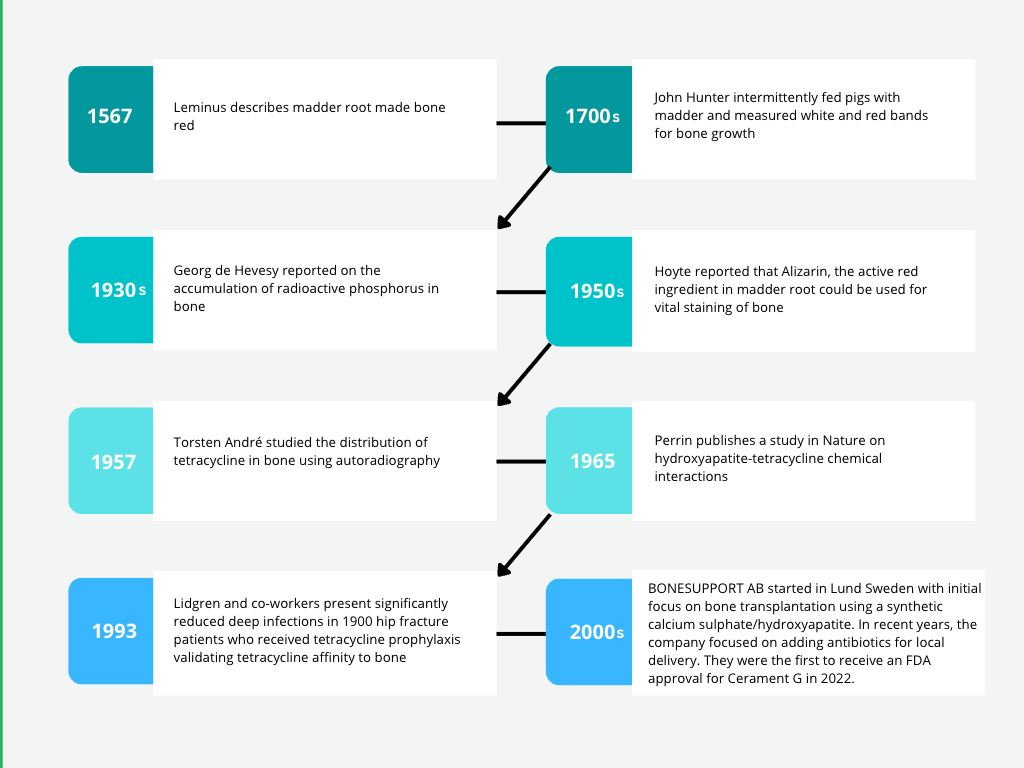
Historical Background
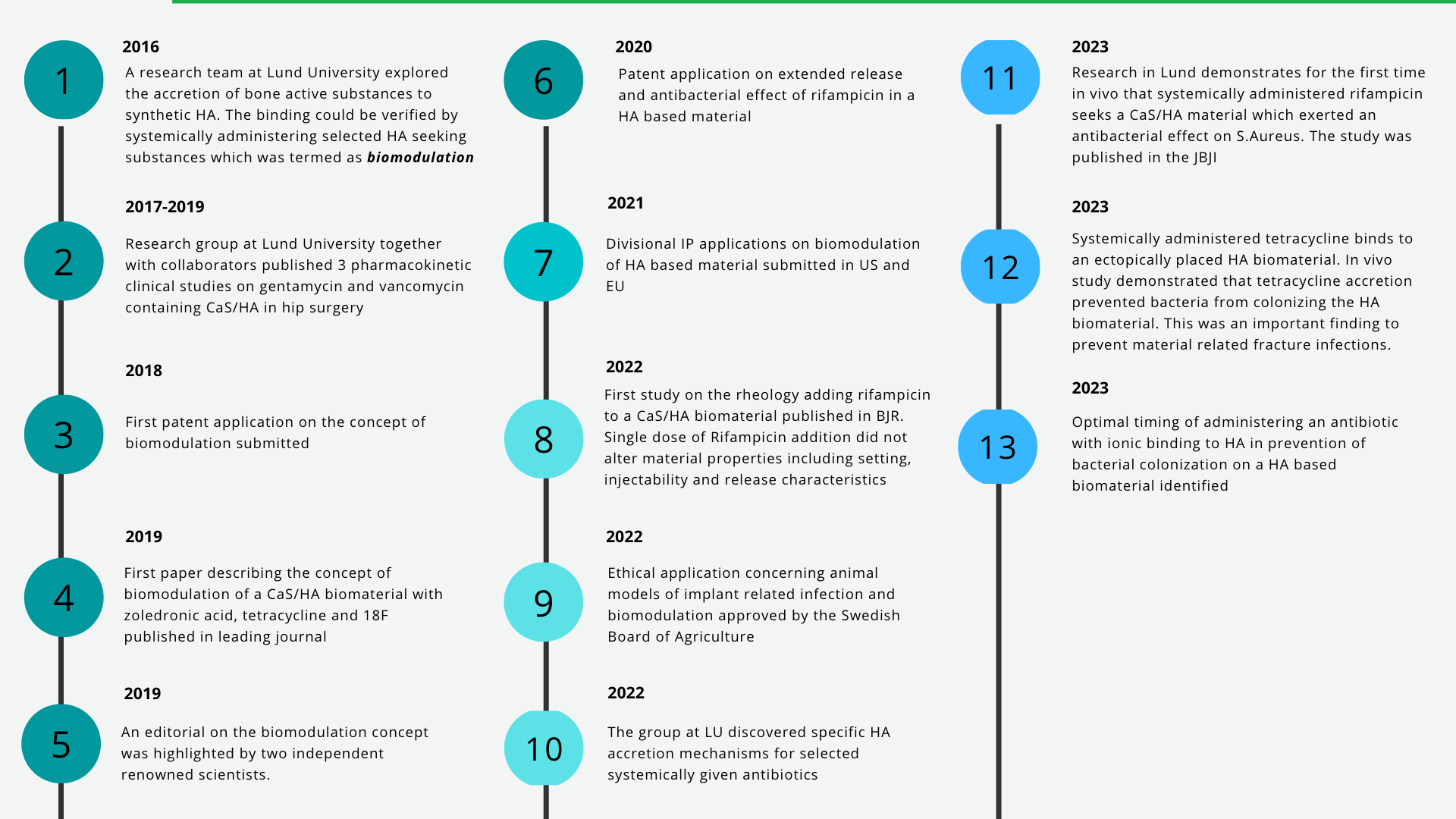
Key Developments